Chemotherapy is a general term for medications used to destroy or stop the growth of cancer cells. Your child’s treatment plan will use the best medicine or combination of medicines available to most effectively combat your child’s specific type and stage of cancer.
 This Children’s Cancer and Chemotherapy video explains how cancer treatments are developed and administered. It’s a great video for caregivers and children to watch together to feel more informed about cancer treatments.
This Children’s Cancer and Chemotherapy video explains how cancer treatments are developed and administered. It’s a great video for caregivers and children to watch together to feel more informed about cancer treatments.
This video was made possible by a grant from AstraZeneca.
Expand all sections Close all sections
Why Chemotherapy Medicines Are Used
Chemotherapy medicines are given for several reasons:
- To treat cancers that respond well to chemotherapy
- To decrease the size of tumors for easier and safer removal by surgery
- To enhance the cancer-killing effectiveness of other treatments, such as radiation therapy
- To control the cancer and enhance the patient’s quality of life
How Chemotherapy Works
Chemotherapy works by interfering with the ability of cancer cells to divide and duplicate themselves. Chemotherapy can be given through the bloodstream to reach cancer cells all over the body, or it can be delivered directly to specific cancer sites.
Each chemotherapy medicine works to prevent cells from growing, by:
- Preventing the copying of cellular components needed for cells to divide;
- Replacing or eliminating essential enzymes or nutrients the cancer cells need to survive; or
- triggering cells to self-destruct.
Often a combination of drugs will be used, with each medicine attacking the cancer cells in a special way. This decreases the chances that cancer cells will survive, become resistant and continue to grow.
Giving Chemotherapy Medicines to a Patient
Chemotherapy is given in different ways depending on the cancer type and the medicines used.
- Intravenously (IV) – injected into a vein
- Intrathecally (IT) – injected into the spinal canal during a lumbar puncture
- Intramuscular (IM) – injected into a muscle
- Intraperitoneal (IP) – injected into the abdominal cavity
- Intracavitary (IC) – injected into a body cavity
- Subcutaneous (sub.q.) – injected into a port just under the skin
- Oral (PO) – as a pill or a liquid to be swallowed
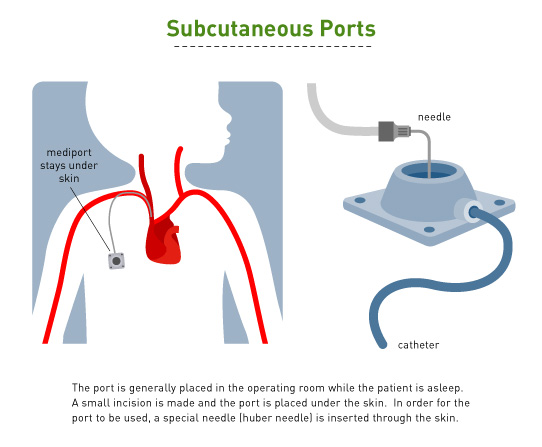
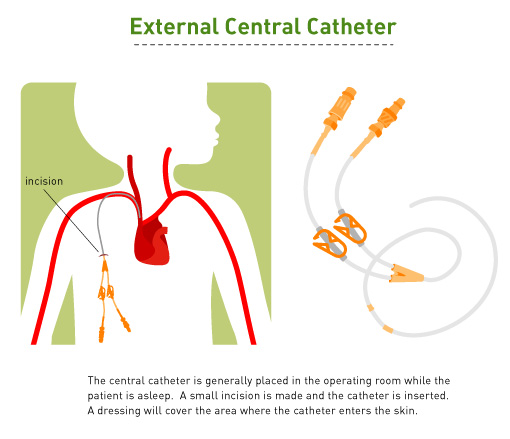
For many patients, the medical team will surgically install a central venous line (catheter) in a vein in the chest (subcutaneous port) or arm before chemotherapy starts. The line will allow treatments to be given and blood samples taken without being “stuck” with a needle. At the end of the treatment, the central line will be removed.
Choosing Chemotherapy Medicines
Many years of research and experience have created successful treatment plans for some types of cancer. For other cancers, research is now underway to find the most effective treatment. Many children are treated according to clinical trial protocols. Each protocol is based on the best available treatment (standard of care) with slight variations that are believed to reduce side effects or improve success. A trial may study two or more different treatment plans, each believed to be effective, with the goal of identifying if one is more effective than the other.
Treatment plans are created using the following guidelines:
- The goal is to maximize the destruction of cancer cells while limiting damage to healthy cells.
- Dosages of the medicines are based on a child’s weight or body surface area.
- The length of treatment depends upon the cancer type and how responsive it is to the chemotherapy.
- Chemotherapy may be stopped if the medicine no longer proves to be effective, or if the child experiences a serious side effect.
- Certain medicines are known to cause permanent side effects after they have been used multiple times. These agents are monitored very closely. Doctors will stop these medicines when the risks of side effects are greater than the potential benefits of continuing treatment.
Tips for Parents
- Review each medicine with your healthcare team, including all potential side effects.
- Discuss what can be done to prevent, lessen, or treat side effects.
- Understand the tests that will be done to monitor side effects.
- Remember that you are the expert on your child. Notify the healthcare team of any changes you notice, or concerns you may have.
Why Does Chemo Cause Side Effects?
Chemotherapy medicines target rapidly dividing cells, including normal ones. Side effects can occur when these normal cells are damaged. Because normal cells are better able to repair the damage or can often be replaced by other healthy cells, side effects are usually temporary.
Factors influencing side effects include:
- The specific chemotherapy medicine
- The dose of the medicine
- The health of the patient
Despite monitoring the effects of chemotherapy very closely, some long-term effects can occur. Some effects may not be known until years after therapy is completed. Therefore, it is important that every patient be followed throughout his or her life by a physician who is aware of the late effects of cancer treatment.
Common Side Effects of Chemotherapy
Anemia
Anemia (a low red blood cell count) can cause excessive tiredness, pale skin color, shortness of breath, irritability, decreased attention span, headaches, and dizziness.
Bruising and Bleeding
Destruction of blood platelets can result in bruising and bleeding. Known as thrombocytopenia, it is caused by a lack of sufficient platelets to form a clot and stop bleeding.
Diarrhea or Constipation
The intestines can be affected by chemotherapy. Proper diet and nutrition can help avoid or reduce these symptoms.
Fever
Fever may be a sign of serious infection. Chemotherapy often temporarily destroys white blood cells, which are the body’s primary defense against infection. If your child has a fever while undergoing chemotherapy treatment, call the doctor right away.
Hair Loss
Some chemotherapy causes hair loss or thinning of the hair. Hair will almost always grow back when treatment is finished, but it may have a different color or texture.
Mouth and Throat Sores
Rapidly growing cells that line the mouth, throat and digestive tract can be temporarily destroyed by chemotherapy medicines. This can cause sores, also called mucositis, which cause minor to severe pain. With time, healthy cells will grow back and the sores will heal.
Nausea and Vomiting
Chemotherapy can cause nausea and vomiting by affecting both the gastrointestinal tract and the message center in the brain responsible for nausea and vomiting. Medicines can be given prior to and during chemotherapy treatments that will help minimize or prevent these symptoms.
Organ Damage
Chemotherapy drugs may affect organs such as the heart, lungs, kidneys, liver, and brain, causing temporary or permanent damage. Some drugs may also affect hearing.
Talk with your child’s healthcare team to understand potential side effects, and to be aware of medical monitoring designed to avoid damage during treatment. You should notify them as soon as there are any changes in your child’s health.
Chemotherapy Medications
It is important to have a basic understanding of the types of chemotherapy that will be used in treatment as well as the most common side effects. Below is a list of the various chemotherapy medications used to treat children’s cancer. Talk to your child’s doctor about the specific medications your child will receive so you can understand how it is given, how it works and potential side effects.
| Medication Name | Also Know As… |
| 5-fluorouracil | 5-FU, Efudix |
| 6-mercaptopurine | 6-MP, Puri-Nethol, Mercaptopurine |
| Aldesleukin | Proleukin, IL-2, Interleukin-2, r-serHuIL |
| Alendronate | Fosamax |
| Allopurinol sodium | Zyloprim, Aloprim |
| Amifostine | Ethyol, Ethiofos, Gammaphos |
| Arsenic trioxide | Trisenox |
| Bleomycin | Bleo, Blenoxane |
| Busulfan | Myleran, Busulfex |
| Carboplatin | Paraplatin, CBDCA |
| Carmustine | Gliadel Wafer, BCNU, BiCNU, bis-chloronitrosourea |
| CCNU | Lomustine, Ceenu |
| Celecoxib | Celebrex |
| Cisplatin | Cis-diamminedichloroplatinum, Platinol-A |
| Cladiribine | CDA, Leustatin |
| Clonazepam | Klonopin, Rivotril |
| Compound 506U | amino-9 bD- arabinofuranosyl 6- methoxy- 9H-purin |
| Cyclophosphamide | CTX, Cytoxan |
| Cyclosporine | Sandimmune, Neoral, Gengraf |
| Cytarabine | Cytosine arabinoside, AraC, Cytosar |
| Dactinomycin | Actinomycin-D, Cosmegen |
| Daunorubicin | Daunomycin, CNR, Cerubidine |
| Deferoxamine | Desferrioxamine, Desferoxamine, DFO, Desferal |
| Dexamethasone | Decadron |
| Dexrazoxane | ADR-529, Zinecard, ICRF-187 |
| Docetaxel | Taxotere |
| Doxorubicin | Adriamycin |
| Ecteinascidin | ET-743 |
| Erwinia asparaginase | Erwinase |
| Etoposide | VP-16, VePeside, Etopophos |
| Fludarabine | Fludara, F-araAMP> |
| Gemcitabine | Gemzar |
| Gemtuzumab ozogamicin | Mylotarg |
| Granulocyte Colony-Stimulating Factor | r-MetHuG-CSF, G-CSF, Filgrastim, Neupogen |
| Granulocyte Colony-Stimulating Factor, Pegylated | Neulasta, PEG-G-CSF, PEG-filigastim |
| Granulocyte Macrophage-Colony Stimulating Factor | rhu GM-CSF, GM-CSF, sargramostin, Prokin, Leukine |
| Hydrocortisone | Cortef, Solu-cortef |
| Hydroxyurea | HU, Hydrea |
| Interferon Gamma-1b | Actimmune, gamma interferon, immune interferon, lymphocyte interferon, rIFN-gamma, T-interferon |
| Interferon-Alpha | alpha-IFN, Intron A, Roferon A |
| Interleukin-4 | IL-4 |
| Isotretinoin | cis-retinoic acid, Accutane |
| L-Asparaginase E. coli | Elspar, Kidrolase, Crasnitin, Leunase |
| Leucovorin Calcuim | LCV, Wellcovorin, citrovorum factor, folinic acid |
| Lymphocyte Immune Globin | Atgam, anti-thymocyte globuline equine |
| MAB Ch.14.18 | |
| Melphalan | L-Phenylalanine Mustard, L-PAM, L-sarcolysin, Alkeran |
| Mesna | Mesnex |
| Methotrexate | MTX, Amethopterin |
| Methylprednisolone | Solu-medrol |
| Mitoxantrone | Novantrone, DHAD |
| Nitrogen mustard | Mechlorethamine hydrochloride, HN2, Mustarge |
| Oprelvekin | Neumega, Interleukin-11 |
| Paclitaxel | Taxol |
| Peg-L-Asparaginase | Pegaspargase, Oncaspar, Polyethlene Glycol conjugated L-Asparaginase |
| Pentostatin | Deoxycoformycin, DCF, Nipent |
| Prednisone | Deltasone, Meticorten, Liquid Pred |
| Procarbazine | Matulane, Natulan |
| PSC-833 | Valspodar |
| R115777 | Farnesyl Protein Transferase Inhibitor, Zarnestra |
| Rasburicase | Elitek, urate oxidase |
| Rebeccamycin Analogue | BMY-27557-14 |
| Rituximab | Rituxan, IDEC-C2B8 |
| Squalamine Lactate | |
| Sulindac | Clinoril |
| Tamoxifen | Nolvadex™, tamoxifen citrate |
| Temozolomide | Temodar™ |
| Teniposide | VM-26 Vumon® |
| Thioguanine | 6-thioguanine, 6-TG |
| Thiotepa | Tepa, Tspa |
| Tirapazamine | |
| Topotecan | Hycamtin |
| Trastuzumab | Herceptin |
| Tretinoin | Vesanoid |
| Urate Oxidase | Rasburicase, UROX, Elitek |
| Vinblastine Sulfate | Velban, Exal, Velbe |
| Vincristine Sulfate | Oncovin, VCR |
| Vinorelbine | Navelbine |
